HARTMANN SCIENCE CENTER

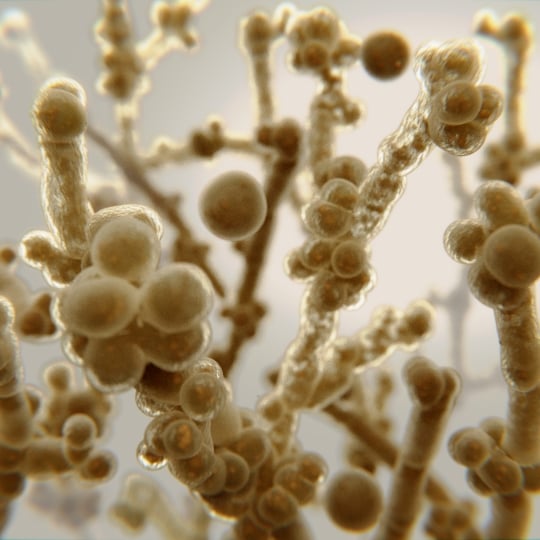
Candidozyma auris is a yeast that can cause serious to fatal infections in humans. C. auris was first discovered in Japan in 2009 in a swab from a patient’s ear, which gave the yeast its name: auris (latin) = ear [1]. Since then, C. auris has been found worldwide. Infections with C. auris tend to occur in immunocompromised people, while healthy people are often only colonised.
C. auris can be resistant to common antifungal drugs (like fluconazole), which can make treatment more difficult. In addition, the yeast can survive on inanimate surfaces for several days or up to three weeks [2]. This increases the risk of indirect transmission through contaminated surfaces and therefore the German National Reference Centre for Invasive Fungal Infections attributes a special role in transmission to medical devices as well as objects and surfaces in the near-patient area [3]. However, direct transmission via hands is also possible.
In 2022, the WHO classified C. auris in the “critical group” of fungal pathogens. Thus, C. auris is one of the top 4 fungal pathogens with highest priority for research, development, and public health actions [4].
In 2024, Candida auris and related species were assigned to the new genus Candidozyma based on detailed phylogenomic and comparative genomic analyses [5].
To prevent the spread of C. auris, in addition to targeted screening procedures, strict hygiene measures are required including proper cleaning and disinfection of surfaces and devices. In general, to inactivate yeasts, a yeasticidal disinfectant tested against Candida albicans (e.g., according to EN 13624) is recommended. However, in case of C. auris, the Centers for Disease Control and Prevention (CDC) recommend using a surface disinfectant with efficacy against spores of Clostridioides difficile [6, 7], while the European Centre for Disease Prevention and Control (ECDC) suggests a disinfectant with fungicidal efficacy [8].
The CDC and ECDC recommendations described above are not substantiated by current scientific literature [9, 10]. Therefore, HARTMANN has tested the two surface disinfectants Mikrobac® forte and Dismozon® plus for their efficacy against C. auris. It was found that the tested exposure times and concentrations, which show a yeasticidal efficacy, are also sufficiently effective against C. auris. C. albicans is thus a suitable representative test organism and the results can be transferred to C. auris as well. In case of an outbreak with C. auris, a yeasticidal disinfectant can therefore be used.
» Necessary spectrum of antimicrobial activity
Yeasticidal
Sources:
Satoh K et al. (2009) Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 53(1):41-4. https://doi.org/10.1111/j.1348-0421.2008.00083.x
Wißmann JE et al. (2021) Persistence of Pathogens on Inanimate Surfaces: A Narrative Review. Microorganisms. 9:343. https://doi.org/10.3390/microorganisms9020343
Nationales Referenzzentrum für invasive Pilzinfektionen (2019) Kurzinfo: Candida auris, https://www.nrz-myk.de/newsticker/kurzinfo-candida-auris-42.html?file=files/content/News/2019_09_23_Candida_auris_final.docx_1.pdf
World Health Organization (2022) WHO fungal priority pathogens list to guide research, development and public health action, https://www.who.int/publications/i/item/9789240060241
(accessed on 14.04.2025).
Liu et al. (2024) Phylogenomic analysis of the Candida auris-Candida haemuli clade and related taxa in the Metschnikowiaceae, and proposal of thirteen new genera, fifty-five new combinations and nine new species. Persoonia 52:22-43.
Centers for Disease Control and Prevention (2020) Candida auris: a drug-resistant germ that spreads in healthcare facilities: a CDC message to infection preventionists, https://stacks.cdc.gov/view/cdc/108262
(accessed on 14.04.2025).
Centers for Disease Control and Prevention – Infection Control Guidance: Candida auris https://www.cdc.gov/candida-auris/hcp/infection-control/ (accessed on 14.04.2025).
European Centre for Disease Prevention and Control (2018) Candida auris in healthcare settings – Europe – first update, 23 April 2018. Stockholm: ECDC, https://www.ecdc.europa.eu/sites/default/files/documents/RRA-Candida-auris-European-Union-countries.pdf
(accessed on 14.04.2025).
Rutala et al. (2019) Susceptibility of Candida auris and Candida albicans to 21 germicides used in healthcare facilities. Infect Control Hosp Epidemiol. 40(3):380-382.
Müller et al. (2020) Investigation of the susceptibility of Candida auris and Candida albicans to chemical disinfectants using European Standards EN 13624 and EN 16615. J Hosp Infect. 105:648-656.
Use surface disinfectants safely.
Always read the label and product information before use.
Mikrobac® forte
Danger
H302 Harmful if swallowed.
H314 Causes severe skin burns and eye damage.
H410 Very toxic to aquatic life with long lasting effects.

Dismozon® plus
Danger
H242 Heating may cause a fire.
H314 Causes severe skin burns and eye damage.
