HARTMANN SCIENCE CENTER Symposium 2026


The choice of workwear plays an important role in everyday medical practice when it comes to patient safety and preventing the spread of germs. Scientific studies clearly show how heavily gowns and other medical garments can be contaminated with pathogens. Pockets and long sleeves are particularly prone to contamination, which is why clinics are increasingly moving away from traditional long-sleeved gowns in favour of short-sleeved tunics.
According to a US study, up to 30% of medical and nursing garments are contaminated with pathogenic bacteria [1]. The degree of contamination obviously depends heavily on the activities performed. Nursing staff who bathed patients or treated wounds had significantly higher contamination rates. The researchers found Staphylococcus aureus or Gram-negative bacteria in 16% of all samples, while enterococci were detected in 3% and multi-resistant pathogens in as many as 6% of samples [1]. In contrast, an Israeli study examined items of clothing for areas particularly susceptible to contamination, such as sleeves or smock pockets. At more than 60%, the proportion of contaminated clothing was higher in the Israeli study, with areas that frequently come into contact with the hands – especially pockets – being particularly prone to bacterial contamination [2].
A review article from 2020 also points out that germs can survive for very long periods on certain textiles. While bacteria can survive on polyester for up to 206 days in individual cases, they usually die on cotton and blended fabrics after about 90 days. Viruses, on the other hand, lose their infectivity on textiles much more quickly and usually remain active for "only" two to four weeks [3]. This highlights the importance of textile hygiene for infection control in patient care.
Despite the hygienic challenges, the classic white doctor's coat still has a special significance: a survey by Johns Hopkins University showed that doctors in white coats are perceived as more experienced, professional and friendly than their colleagues in fleece or softshell jackets [4]. The white coat therefore has a positive effect on patient confidence. Nevertheless, clear hygiene rules are needed to make the use of coats safer within a defined framework. This includes, for example, changing coats daily, not wearing them outside the healthcare facility, and taking them off and hanging them up properly when working directly with patients [3,5].
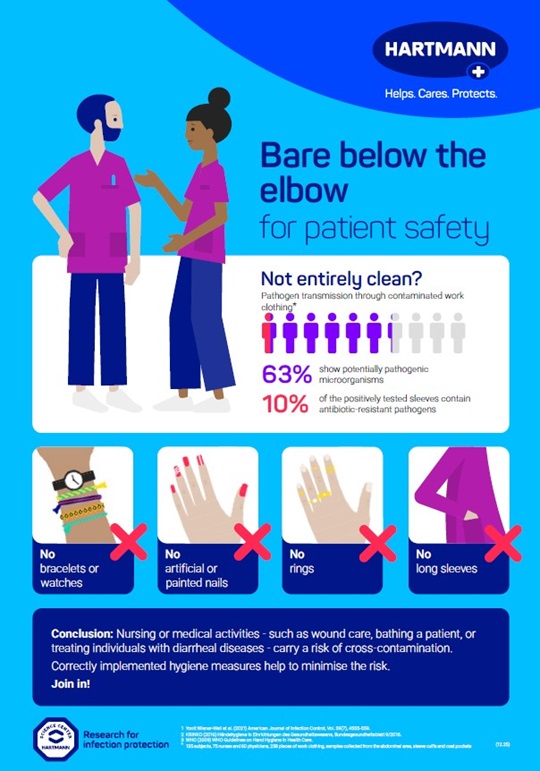
Even if responsible use of the gown is assumed, hygienic hand disinfection with long sleeves can hardly be effective due to the risk of recontamination. Short-sleeved clothing is therefore an important part of infection prevention in many medical areas. In addition to choosing a suitable hand disinfectant, bare forearms are a prerequisite for correct and complete hand disinfection. The standard hygiene requirements for medical and nursing workwear also include [6,7]:
This concept – known internationally as "bare below the elbow" – reduces the risk of pathogens sticking to hands and forearms or being transmitted through clothing.
Workwear in the healthcare sector must therefore meet various requirements: it should support the highest standards of hygiene while also inspiring confidence. Exposed forearms combined with good hand hygiene remain a key principle for providing the best possible protection for patients and staff.
You can download the poster "Bare below the elbow for patient safety" here.
Use surface disinfectants safely. Always read the label and product information before use.