HARTMANN SCIENCE CENTER

Healthcare-associated infections and sepsis mortality are important public health problems. It has been shown many times that strategies to reduce HAI can significantly improve the situation. In the US, since 2012, a reform of the healthcare system has allowed hospitals to implement infection prevention strategies with incentive payments to reduce both HAIand sepsis mortality. The authors of a study published in 2021 took the opportunity to conduct a prospective observational study on quality improvement in a 770-bed public academic hospital in Texas (USA) from 2013 to 2017 [1]. Because of its participation in the government-funded programme, the hospital was able to implement a predefined set of interventions. These included an awareness campaign (e.g. newsletters, screensavers, sharing of surveillance data), clinician engagement (e.g. lunch seminars, focus group meetings), implementation of HAI and sepsis bundles, training of clinical staff on the bundles, training of managers and staff in quality improvement methods, and clinical decision support through electronic health records.
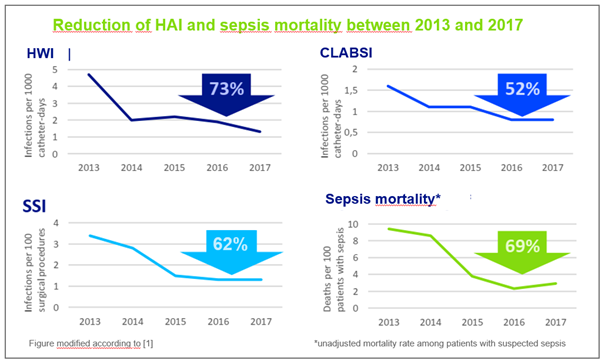
For the 5-year study period, vascular catheter-associated bloodstream infections (BSI), catheter-associated urinary tract infections (UTI), postoperative wound infections (surgical site infections, SSI) and sepsis mortality were defined as primary endpoints. Data were collected by trained hygienists by reviewing electronic medical records. This showed that overall infection rates were significantly reduced over the period. For example, 73% fewer UTIs, 52% fewer BSIs and 62% fewer SSIs were recorded in 2017 than in 2013, and the unadjusted mortality rate for patients with suspected sepsis was reduced by 69%. All these effects were statistically significant.
In addition to the data on the primary endpoints, various processes such as compliance withbundles of measures, hand hygiene and safety culture were also regularly monitored. This showed that compliance with the bundles of measures and hand hygiene improved throughout the study period. While the average monthly consumption of hand disinfectant was 703 litres before the survey, it rose to a plateau of 2,917 litres during the study and reached as high as 3,631 litres in subsequent years. In addition, the perceived patient safety climate of health workers improved significantly, as regular surveys showed.
Sources:
Sreeramoju P et al. (2021) Results and lessons from a hospital-wide initiative incentivised by delivery system reform to improve infection prevention and sepsis care. BMJ Open Qual 10: e001189. https://doi.org/10.1136/bmjoq-2020-001189